Shingles

-
- 20%. people have shingles at least once in their lifetime, and the incidence is rising.
- Varicella zoster virus can cause two different diseases: chickenpox and shingles.
- When a person gets chickenpox, the virus continues to live in the body (in the nerve nodes) without causing any symptoms, but when it becomes active it can cause herpes zoster.
- If you have never had chickenpox and have not been vaccinated against it, it is possible to get chickenpox from a person with shingles through direct contact with the rash or through inhalation of Varicella zoster virus.
- Approximately 1-6% of people develop recurrent shingles.
- Shingles should be distinguished from herpes zoster, rosacea, acute eczema, and the disseminated form from chickenpox.
Risk groups
-
- Shingles can affect people of all ages, but is most common in people over 50
- It is also more common in people of all ages, with weak immune systems (e.g. Oncology patients; patients with chronic, autoimmune diseases (rheumatoid arthritis, scarlet fever, etc.) – who are treated with systemic steroids, tumour necrosis factor (TNF)-alpha inhibitors, sphingosine-1-phosphate (S1P) receptor inhibitors, Janus kinase (JAK) inhibitors.
- People living with HIV and AIDS.


-
- A person with chickenpox, less commonly shingles
- Varicella zoster virus is transmitted by droplets in the air or by contact (touching the rash).
- Children can get chickenpox from a person with shingles, and vice versa
Provocative factors
-
- older age (>50 years)
- colds
- stress
- infections
- Injuries
- contact with a person with chickenpox or shingles
- UV rays
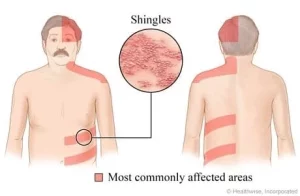
Localisation
-
- 50% are intercostal (nn. intercostales, n. thoracicus) nerves in the thoracic and dorsal regions.
- 20% n.trigeminus; n.VII and n.VIII in the face.
- Less common are segments of the neck, lumbar spine and sacrum.
- In immunosuppression, may spread outside the segment to be anaesthetised
The clinical picture depends on the patient’s age and health status, and the affected area (dermatome). A dermatome is an area of skin innervated by a single spinal nerve.
-
- 3-5 d. general malaise, fatigue, fever, pain and burning in the area of the future rash before the skin is rubbed;
- Reddish spots-painful unilateral erythema (redness) – grouped papules, vesicles with clear fluid (12-24 hours) following the course of a nerve;
- Pimples – scabs (7-12 days)
- In severe cases: bloody-serous, gangrenous rashes
- Burning, pain, itching
Complications
-
- Skin: secondary bacterial infection may be present, with scarring during healing;
- Eyes: conjunctivitis, episcleritis, uveitis, keratitis, iridocyclitis (glaucoma), chorioretinitis (AIDS), retrobulbar neuritis, vasculitis, optic nerve atrophy. Herpes zoster ophthalmicus – lesion r. ophtalmicus n. Trigemini, vesicles appearing on one side of the eyelids and nose, affecting the cornea.
- Nervous system: encephalitis, meningitis, granulomatous arteritis, segmental paresis, N. facialis paresis, auditory nerve damage; postherpetic neuralgia is a very common complication. Pain without rashes, lasting for months or years. Hypo- or hyperaesthesia may be present and often requires medical treatment. a neurologist or pain medicine doctor for advice on pain relief.
- Internal organs: pneumonia, oesophagitis, myocarditis, enterocolitis, pancreatitis, arthritis.
Diagnostics
-
- Diagnosis is usually made by questioning and physical examination
- Laboratory tests can be used to confirm a definitive diagnosis if necessary:
-
- Polymerase chain reaction (PCR)
- Virological testing – growing the virus in infected cell cultures
- Direct immunofluorescence – to detect Varicella-zoster virus antigen
- Serological tests – IgM and IgG (Anti Varicella Zoster IgG and IgM)
- The material for testing is taken from the rash (vesicles).
-


Treatment recommendations
At the first sign of the disease, it is recommended to consult a doctor immediately. Do not self-treat, but consult your family doctor or a dermatovenereologist who will draw up the most appropriate treatment plan for you – this is the only way to avoid complications.
-
-
- Antiviral treatment is effective in reducing pain and symptom duration if started within 72 hours from the start of symptoms.
- More than 72 hours later the medicine can be given if new rashes appear.
- Do not rub, scratch or disinfect rashes to prevent them from growing
- Antiviral treatment is not indicated if the rashes are covered with scabs
- Other measures: rest, pain relief (cold, antiviral ointments, local steroids, emollients (creams, lotions, ointments – from the pharmacy), antiseptics, antibiotics in case of a secondary bacterial infection, B vitamins).
-
- In postherpetic neuralgia, it is important to:
-
- early antiviral treatment
- use of local anaesthetic
- a neurologist’s advice on how to relieve the pain (medications: non-steroidal anti-inflammatory drugs (NSAIDs), although usually not very effective, tricyclic antidepressants, antiepileptic drugs; non-medications: transcutaneous electrical nerve stimulation or acupuncture, injections into the affected areas).
-
Sick leave
-
- If the rash is on your face, don’t return to work until the scab has formed (~7-10 days)
- If the rash is in an area that you can cover (e.g. with a gauze bandage or clothes), you can return to work when you feel well.
- If you work in a healthcare facility (e.g. hospital, medical centre, nursing home), check with your doctor when it is safe to return to work.
Prevention
-
- Vaccination against Varicella zoster virus is recommended;
- Getting vaccinated can reduce your chances of developing shingles and postherpetic neuralgia
- The vaccination is recommended for adults over 50 years of age, but younger people can also be vaccinated, especially if their immune system is weaker than usual.

1. Harbecke R; cohen J I. Oxman M N. Herpes zoster vaccines. The Journal of infectious diseases. 2021; 224.Supplement_4: S429-S442.
2. Koshy, E., Mengting L., Kumar H., Jianbo W. Epidemiology, treatment and prevention of herpes zoster: A comprehensive review.
Indian Journal of Dermatology, Venereology and Leprology
. 2018;
84
(3).
3. Saguil A, Kane S F, Mercado M G, Lauters R. Herpes zoster and postherpetic neuralgia: prevention and management. American family physician, 2017; 96.10: 656-663.
Psoriasis
A common, chronic, inflammatory, recurring skin disease that affects 2-3% of the population. Psoriasis can start at any age, and is most often found in adults.
Juvenile plantar dermatosis
a disease characterized by localized damage to the feet. JPD usually occurs in children between the ages of 3 and 14 who are prone to atopy or have atopic dermatitis
Skin Conditions in Newborns: Causes, Symptoms, and Care Tips
Skin conditions like rashes, eczema, and cradle cap are common in newborns. Proper skin care is essential for managing and preventing these issues. Learn how to care for your baby’s delicate skin and address common skin conditions effectively.
iDerma
MB iDerma
Fabijoniškės g. 99, Vilnius
+370 670 70 822
[email protected]




